Table of Contents
A.J. took two small hits off a cannabis vape pen, a common ritual with his morning coffee. Moments after exhaling, a transfigured, kaleidoscopic version of the world emerged before his eyes.
“Some colors are seeping into the other colors,” the 30-year-old said, gesturing across his art-filled living room in Yorba Linda. “In that Persian tapestry on the wall, the flowers are flowing like the wind, back and forth, and the centerpieces of the horses and other animals, they’re stagnant still but I can feel them kind of moving, almost like a gallop.”
A.J. — who requested anonymity to discuss his drug use and medical history — was on no other mind-altering substances beyond the caffeine in his mug. The fantastical visions, which he’s come to expect and in some ways even enjoy, were a lingering effect of past drug use. They’re a manifestation of a rare condition called hallucinogen persisting perception disorder, or HPPD, which has puzzled psychiatrists and researchers and raised alarms as psychedelic drugs have become more mainstream for both therapeutic and recreational use.
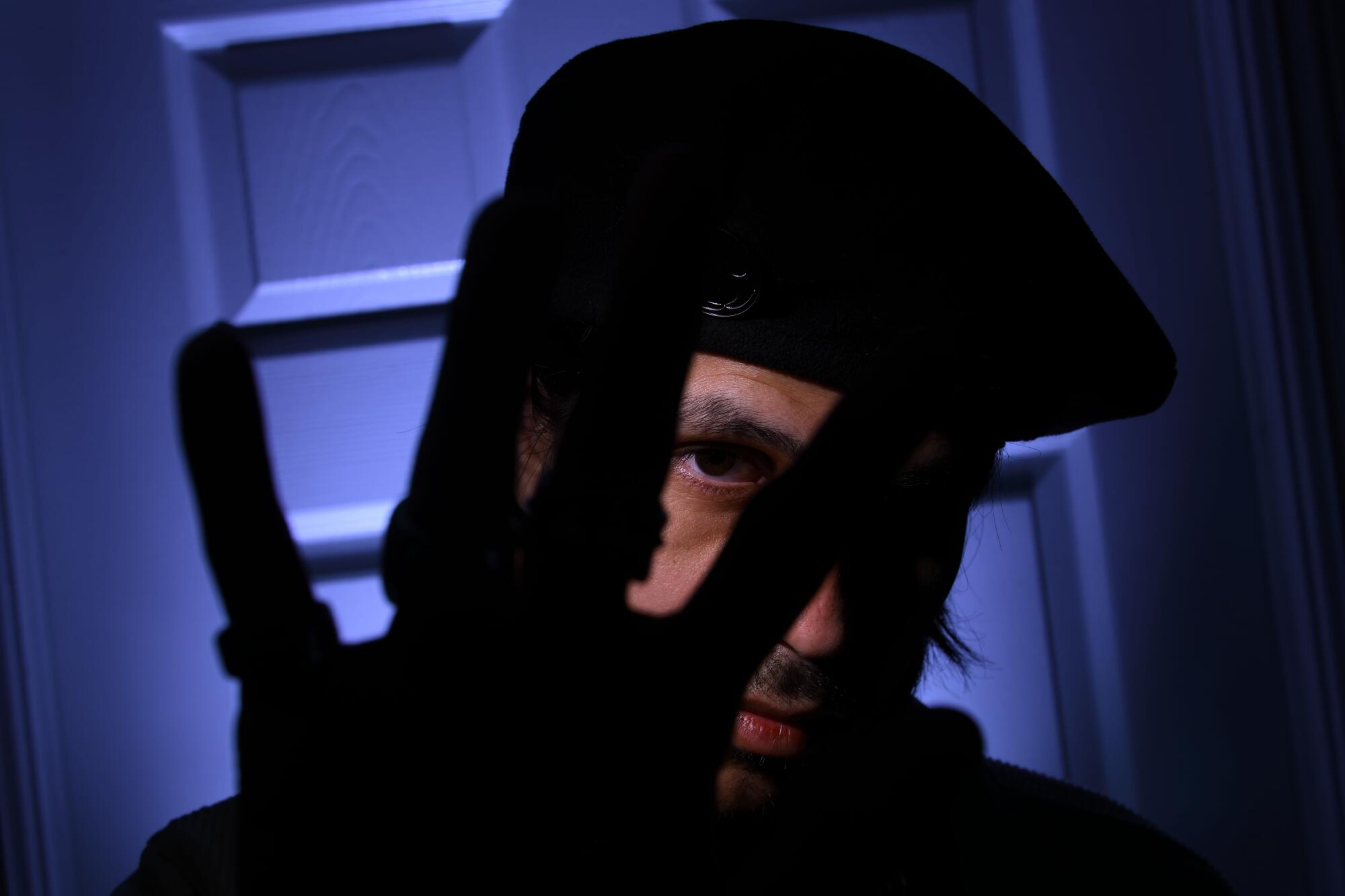
A.J., a 30-year-old who requested anonymity to discuss his drug use and medical history, said he suffers from hallucinogen persisting perception disorder, a rare condition brought on by the use of psychedelic drugs.
(Paul Rodriguez / For The Times)
LSD and other hallucinogens have long been said to cause flashbacks for some heavy users, but HPPD is a unique phenomenon. It’s a lasting condition defined by a range of symptoms straight out of the “Electric Kool-Aid Acid Test.”
Psychiatrists, researchers and more than a dozen people with HPPD said in interviews that the mysterious and beguiling condition may be more common than currently known.
Some who suffer from HPPD develop the disorder after years of using hallucinogenic drugs such as LSD and psilocybin mushrooms. For others, just a single psychedelic experience can bring on its lasting effects. In a smaller number of cases, it has been triggered by MDMA and even cannabis alone.
Some with the condition live for years with frequent or near-constant visual aberrations. Others experience mild symptoms that pass after a few months. Many develop serious psychological and mental conditions, including anxiety, depression and dissociation from reality.

A.J. said that at their most intense, the symptoms of hallucinogen persisting perception disorder can make him feel as if he’s experiencing a full-on psychedelic trip.
(Paul Rodriguez / For The Times)
At its most severe, HPPD can destroy people’s lives or impair their basic faculties. Some lose jobs or fail out of school. A.J.’s visual perception was so affected that he had to relearn how to write and drive.
Many professionals who treat people with HPPD say they don’t want to discourage safe and informed use of psychedelics. But they warn that the condition can be life-changing, and that people should know the risk before dabbling in hallucinogens. Like any drug, doctors say, these powerful substances have side effects; for some, those effects don’t subside, and they are left to live for months or years with HPPD.
“Informed consent would mean full awareness of the risks, and I don’t think that’s happening right now,” said Sara Ouimette, a licensed psychotherapist in Oakland who has treated more than 20 people with the condition. “We’re only going to see more cases, unfortunately, as people are doing psychedelics like the Wild West.”
‘The brain-mind interface’
A former Harvard Medical School psychiatry professor and one of the world’s leading authorities on HPPD, Dr. Steven Locke, described the condition as “really at the brain-mind interface.”
Like the brain itself, much about the disorder remains a mystery.
The first description in a mainstream medical journal of the phenomenon was published more than 65 years ago, Locke said, and since then there have been sporadic news reports and psychological studies. It was first included as a diagnosis in the Diagnostic and Statistical Manual of Mental Disorders, or DSM, more than 30 years ago — yet many psychiatrists and other clinicians still have no idea the disorder exists.
After Dr. Henry Abraham, considered the grandfather of HPPD research, retired in 2017, Locke took on many of his patients. Since then, Locke has developed a general working theory of what causes HPPD and how it works.
“Long after the drug has left the body, there’s nevertheless a persistence of abnormal activity in the brain,” he said. Exposure to psychedelics such as LSD and psilocybin is believed to be able to alter parts of the brain, he said.
On Sunday, one of Locke’s colleagues will present the findings of a recently completed survey at the annual conference of the American Psychiatric Assn. in New York.
Locke and other researchers from Harvard, Columbia and Johns Hopkins universities and the New York State Psychiatric Institute conducted an online survey of more than 650 people who self-identified as having experienced HPPD symptoms. The results present one of the most complete pictures to date of the scope of the perplexing condition and efforts to treat it.
Nearly half of the respondents reported taking multiple “precipitating drugs,” about one-fifth said they took only LSD, roughly 13% took only psilocybin mushrooms, and 5.5% listed only cannabis. The average age of the survey’s respondents was 28, and more than 8 in 10 identified themselves as white — about the same proportion as were male.
There appears to be a correlation with previous mental health diagnoses. More than half of the survey’s respondents reported that they had previously struggled with anxiety, panic attacks, depression, post-traumatic stress disorder and other conditions.
What’s baffling is that some people can develop permanent-trip symptoms after using drugs only a few times, while others emerge from years of frequently dosing on LSD and mushrooms with no lingering issues.
Studies have found that 2% to 4% of people who experiment with psychedelics will develop HPPD, and many of them will have short-lived or mild cases. Some clinicians put the proportion far lower, though others caution that there probably is a significant undiagnosed population.
Some experts believe a bad drug trip can inflict severe trauma that leaves people with a condition akin to PTSD. Dr. Wesley Ryan, who has treated about a dozen people with HPPD at his psychiatric practice in Marina del Rey, said such patients often experience depersonalization and derealization. They feel like they are witnessing their own life from the outside or that nothing is real.
“Maybe the wires get crossed in a way that they shouldn’t have, and that’s why they get these persistent visual hallucinations,” Ryan said.
Experts say a person’s mindset and the setting in which they take hallucinogens are key to avoiding negative experiences. Being with trusted people in a safe, comfortable location can go a long way toward avoiding a bad trip that could potentially trigger the onset of HPPD.
Many who develop symptoms experienced trauma as children, said Carol Gilson, a Texas-based psychotherapist and licensed clinical social worker supervisor, who has treated about two dozen patients with the disorder.
In psychedelic therapy, the drugs are used to help people unlock feelings and work through past trauma. But in non-therapeutic environments, Gilson said, there’s a risk the experience “might amplify a past traumatic experience or your greatest fear.”
The psychotherapist Ouimette agreed, adding, “If they’ve had that childhood trauma, as opposed to being healing, it can kind of get stuck.”
When trauma resurfaces during a psychedelic experience, Gilson said, the result for some is “the fight or flight system gets activated and it doesn’t get turned off.”

A.J. said he’s come to expect and in some ways even enjoy his HPPD symptoms.
(Paul Rodriguez / For The Times)
The detrimental effects can last decades.
“I have quite a few patients who’ve had their symptoms for 10 years or more,” Locke said. “Those people have a fair amount of regret because they feel that they’ve broken their brains.”
‘Everything’s melting, everything’s morphing’
Adonai Vargas was 14 years old when he first developed HPPD. He was already an experienced hallucinogen user who had experimented with the powerful compound DMT and says he was taking LSD once a week “like a dumb teenager.”
Now he’s 21 years old and entirely sober, save for the benzodiazepines he takes for limited relief when he can’t handle his ceaseless symptoms.
He used to enjoy books but hasn’t been able to read anything longer than a few pages since the symptoms began. He often uses voice to text on his phone because his perception of words and letters is so scrambled.
“I’m still seeing visuals all the time, constantly,” he said last month during a phone interview from Miami. “It’s like you took three tabs of acid, straight up. Everything’s melting, everything’s morphing, geometric patterns everywhere, everything breaking and cutting and splitting…. It never stops from when I wake up to when I go to bed.”
Vargas’ case is extreme, but researchers and clinicians who treat patients with the condition say he’s not unique.
For Vargas, it all began with what he termed “a nightmare experience with a bad trip.” As a 14-year-old in his room in his childhood home in Albuquerque, he took two tabs of what he described as “really strong acid” that he bought off the dark web.
“Out of nowhere, I got sent to a hellish dimension I don’t how to explain in words,” he said. “Time didn’t exist, infinite torture, chainsaws ripping through my body, thousands of my worst fears I didn’t know I had were happening to me.”
Vargas called out for his mother, who found him in a delusional state and called the police. He blacked out and was taken to a hospital for psychiatric evaluation and treatment.
Since then, he’s struggled to find anyone who knows anything about HPPD. Sometimes, he thought doctors’ efforts did more harm than good, such as when he was prescribed antipsychotics and antidepressants that seemed to exacerbate his symptoms.
The lack of awareness and understanding among medical professionals is a common complaint of those who suffer from HPPD. With research into the condition still in its infancy, the internet has filled a void for those seeking help.
Vargas said he found support and solidarity last month on the HPPD subreddit when his symptoms were at their worst. Dozens of commenters shared their own stories of overcoming the condition and offered resources and treatment recommendations, such as meditating or medicating with antidepressants or vitamins.
He found the responses heartening and is now seeking a way to either eliminate his symptoms or learn to live with them. He’s since begun meditating and plans to see a new psychiatrist soon.
It can be a long journey back to the unaltered world, and some never make it. But an HPPD diagnosis does not necessarily mean being doomed to suffer from the disorder’s most disorienting and debilitating effects.
‘Doctors need to know this is a thing’
Will Higgins sat looking out at the Santa Rosa Mountains beyond his backyard in La Quinta as heavy gusts blew cushions off furniture and covered everything in a layer of fine sand. He first developed HPPD in 2013, he said, three days after he took what he was told was LSD but now believes was a different, more dangerous synthetic hallucinogen.

Will Higgins, 33, shown reflected through his dining room window in La Quinta, said he developed hallucinogen persisting perception disorder after taking a strong psychedelic drug.
(Gina Ferazzi / Los Angeles Times)
“Who I was disappeared overnight. There’s a core of me that obviously was still there, but it just blew me away like that wind,” the 33-year-old said. “I had to rebuild myself. It took a long time.”
Higgins was days away from starting classes at a new college, where he had recently transferred to study ceramics, but the initial symptoms were overwhelming. Initially, he said, he suffered “near-constant panic attacks” and saw “wavy gasoline colors” from the moment he woke up. He felt like his IQ had plummeted and he was rendered almost incapable of reading and writing. Everything around him, he said, “was growing and shrinking … like ‘Alice in Wonderland.’”
For two years, he had no idea that his condition had a name. But over time, Higgins said, he discovered that living cleanly and spending time in nature reduced the negative effects. He also found relief from two medications, a mood stabilizer called Lamictal and an anticonvulsant called Keppra. Today, he no longer experiences much in the way of HPPD-induced visual effects.

Will Higgins, shown with his girlfriend and their dog Moxie, said HPPD initially rendered him almost incapable of reading and writing. But now, he said, living cleanly and spending time in nature has diminished the disorder’s negative effects.
(Gina Ferazzi / Los Angeles Times)
More than 90% of the people who responded to Locke’s online survey reported that they had taken medication or supplements or undergone other mental heath treatment for their HPPD symptoms. Benzodiazepines such as Xanax showed the highest success rate, with 58% of those who took them reporting that their symptoms improved. Antidepressants, meanwhile, had a positive impact on only 11% of respondents’ symptoms, while a third of those who took them said their symptoms worsened.
A few HPPD sufferers who spoke with The Times said they have tried taking more psychedelics in pursuit of a way back to their pre-trip existence. Gilson, the Texas psychotherapist, said the visual changes she experienced after experimenting with hallucinogens in high school “mostly resolved themselves” after she completed psychedelic therapy years later. They haven’t gone away entirely, but she considers the low-grade lingering effects “a gift.”
“I’m looking at a tree in my backyard right now, and the way the sun is shining, some leaves sparkle while others are in the shade,” she said, describing a “kaleidoscopic” effect. “I don’t see it as something that’s scary or anything wrong. It’s just a moment of the door of perception being opened.”
Nearly half of the respondents to Locke’s survey who tried yoga, meditation, neuro-feedback and other nonmedical treatments reported that they were helpful. For many, simply coming to terms with its negative effects can be an effective way to reduce them.
Samuel Smith, 21, said he already suffered from depression and anxiety before he developed HPPD after a single time ingesting a relatively moderate dose of about two grams of psilocybin mushrooms. Now, he takes an anti-seizure drug called Lamotrigine each day, which he said has “dumbed down the visuals a lot, and it got rid of the geometric patterns and colors and stuff when I closed my eyes.”
He initially experienced crushing anxiety over the condition, but ultimately found that limiting the attention he dedicated to its worst effects helped bring them under control.
“You’ve got to learn to ignore it and live with it,” the Henderson, Nev., resident said. “As someone who had it pretty bad, I was able to get over it, and once you get over it, that helps with reducing the visuals.”
Higgins now dedicates much of his time to research and helping people with the condition better understand the diagnosis and how to treat it.
“This disorder has stigma and shame attached to it. People often dismiss people with HPPD as druggies,” he said. “We deserve the same amount of caring and attention as people with any serious life-altering condition. … For that to happen, doctors need to know this is a thing.”

